Purpura is a condition characterized by the appearance of purple or red spots on the skin, which are caused by bleeding underneath the skin. These spots are typically small and may be accompanied by other symptoms such as fatigue, fever, and joint pain. Purpura can be caused by various factors, including underlying medical conditions, medications, and certain infections. Treatment options for purpura depend on the underlying cause and may include medication, lifestyle changes, and supportive care. In this article, we will explore the causes, treatment options, and management strategies for purpura.
Purpura Symptoms
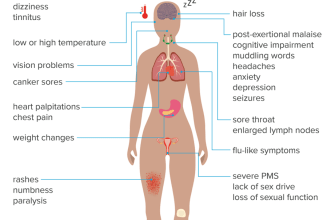
The symptoms of purpura can vary depending on the underlying cause and the severity of the condition. Common symptoms include:
- Appearance of purple or red spots on the skin
- Easy bruising
- Fatigue
- Fever
- Joint pain
- Nosebleeds
- Bleeding gums
If you experience any of these symptoms, it is important to consult a healthcare professional for a proper diagnosis and appropriate treatment.
Purpura Causes
There are several potential causes of purpura, including:
- Platelet disorders: Conditions that affect the production or function of platelets, such as immune thrombocytopenic purpura (ITP) or thrombotic thrombocytopenic purpura (TTP), can lead to purpura.
- Blood vessel disorders: Certain conditions that affect the blood vessels, such as vasculitis or Henoch-Schönlein purpura, can cause purpura.
- Medications: Some medications, such as blood thinners or nonsteroidal anti-inflammatory drugs (NSAIDs), can increase the risk of bleeding and purpura.
- Infections: Certain infections, including meningococcal infection or viral infections like dengue fever, can cause purpura.
- Underlying medical conditions: Purpura can be a symptom of underlying medical conditions, such as leukemia, liver disease, or autoimmune disorders.
It is important to identify the underlying cause of purpura in order to determine the most appropriate treatment approach.
Purpura Treatment
The treatment of purpura depends on the underlying cause and may involve a combination of medication, lifestyle changes, and supportive care. Some common treatment options include:
- Medication: Depending on the cause of purpura, medications such as corticosteroids, immunosuppressants, or antibiotics may be prescribed to manage the condition.
- Lifestyle changes: Making certain lifestyle modifications, such as avoiding activities that may increase the risk of bleeding or injury, can help manage purpura.
- Supportive care: Supportive care measures, such as applying cold compresses to reduce swelling or using pain relievers to alleviate discomfort, may be recommended.
It is important to follow the treatment plan prescribed by your healthcare professional and attend regular follow-up appointments to monitor your condition.
Types of Purpura
There are different types of purpura, each with its own specific characteristics and underlying causes. Some common types of purpura include:
Immune Thrombocytopenic Purpura (ITP)
ITP is a condition characterized by a low platelet count, which can lead to purpura. It is an autoimmune disorder in which the immune system mistakenly attacks and destroys platelets. Treatment options for ITP may include medication to increase platelet count or surgery in severe cases.
Henoch-Schönlein Purpura
Henoch-Schönlein purpura is a type of vasculitis that primarily affects children. It is characterized by purpura, joint pain, abdominal pain, and kidney inflammation. Treatment for Henoch-Schönlein purpura may involve medication to reduce inflammation and manage symptoms.
Thrombotic Thrombocytopenic Purpura (TTP)
TTP is a rare blood disorder characterized by the formation of blood clots in small blood vessels throughout the body. It can lead to purpura, as well as other symptoms such as fever, neurological abnormalities, and kidney dysfunction. Treatment for TTP typically involves plasma exchange or medication to suppress the immune system.
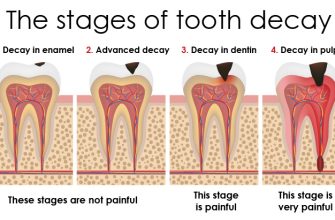
Purpura Diagnosis
Diagnosing purpura involves a thorough evaluation of the patient’s medical history, physical examination, and laboratory tests. The healthcare professional may perform blood tests to assess platelet count, clotting factors, and other relevant parameters. In some cases, a skin biopsy may be performed to confirm the diagnosis and rule out other potential causes of purpura.
Purpura Prevention
While it may not always be possible to prevent purpura, there are certain measures that can help reduce the risk. These include:
- Avoiding activities that may increase the risk of injury or bleeding
- Managing underlying medical conditions effectively
- Following a healthy lifestyle, including a balanced diet and regular exercise
- Discussing the potential side effects of medications with your healthcare professional
It is important to consult a healthcare professional for personalized advice on preventing purpura based on your specific circumstances.
Purpura Management
Managing purpura involves a combination of treatment, lifestyle modifications, and regular monitoring. Some strategies for managing purpura include:
- Following the prescribed treatment plan, including taking medications as directed
- Adopting a healthy lifestyle, including a balanced diet and regular exercise
- Attending regular follow-up appointments with your healthcare professional
- Monitoring for any changes in symptoms or the appearance of new spots
- Seeking immediate medical attention if there are signs of bleeding or other complications
By actively managing purpura, individuals can help minimize the impact of the condition on their daily lives and overall well-being.
Purpura Risk Factors and Complications
There are certain risk factors that may increase the likelihood of developing purpura. These include:
- Age: Certain types of purpura, such as Henoch-Schönlein purpura, are more common in children.
- Underlying medical conditions: Having certain medical conditions, such as autoimmune disorders or liver disease, can increase the risk of developing purpura.
- Medications: Taking certain medications, such as blood thinners or NSAIDs, can increase the risk of bleeding and purpura.
Complications of purpura can vary depending on the underlying cause and may include:
- Excessive bleeding
- Organ damage
- Kidney problems
- Neurological abnormalities
It is important to seek medical attention if you experience any complications or worsening of symptoms.
Purpura Prognosis
The prognosis for individuals with purpura depends on the underlying cause, the severity of the condition, and the effectiveness of treatment. In many cases, purpura can be managed effectively with appropriate treatment and lifestyle modifications. However, some types of purpura may have a more chronic or recurrent course. It is important to work closely with your healthcare professional to develop a personalized treatment plan and monitor your condition regularly.
In conclusion, purpura is a condition characterized by the appearance of purple or red spots on the skin, which can be caused by various factors. Treatment options for purpura depend on the underlying cause and may include medication, lifestyle changes, and supportive care. By understanding the symptoms, causes, and treatment options for purpura, individuals can take proactive steps to manage their condition and improve their overall well-being.