Diabetes insipidus is a rare condition that affects the body’s ability to regulate fluid balance. It is characterized by excessive thirst and the production of large amounts of diluted urine. In this article, we will explore the causes, symptoms, and treatment options for diabetes insipidus, as well as the different types of the condition and its management.
Understanding Diabetes Insipidus
Diabetes insipidus is not related to the more common form of diabetes, known as diabetes mellitus. While diabetes mellitus is characterized by high blood sugar levels, diabetes insipidus is caused by a deficiency of antidiuretic hormone (ADH), also known as vasopressin. ADH is responsible for regulating the amount of water reabsorbed by the kidneys.
Causes of Diabetes Insipidus
There are several potential causes of diabetes insipidus. The most common cause is damage to the hypothalamus or pituitary gland, which can occur due to head injuries, tumors, or certain genetic conditions. In some cases, diabetes insipidus may be caused by a failure of the kidneys to respond to ADH, known as nephrogenic diabetes insipidus. This can be a result of certain medications, kidney disease, or genetic factors.
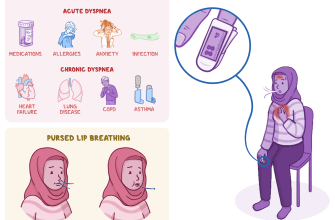
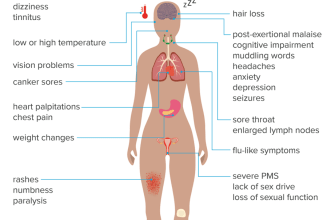
Symptoms of Diabetes Insipidus
The main symptom of diabetes insipidus is excessive thirst, also known as polydipsia. Individuals with the condition may feel the need to drink large amounts of water throughout the day and may wake up multiple times during the night to urinate. Other symptoms can include:
- Excessive urination (polyuria)
- Dehydration
- Weakness
- Fatigue
- Weight loss
If left untreated, severe dehydration can occur, leading to complications such as electrolyte imbalances and kidney damage.
Diagnosis of Diabetes Insipidus
If you are experiencing symptoms of diabetes insipidus, it is important to seek medical attention for a proper diagnosis. Your doctor will likely perform a series of tests, including:
- Water deprivation test: This test involves restricting fluid intake to determine how the body responds and whether urine becomes more concentrated.
- Blood and urine tests: These tests can help measure hormone levels and assess kidney function.
- Magnetic resonance imaging (MRI): An MRI may be ordered to examine the hypothalamus and pituitary gland for any abnormalities.
Treatment for Diabetes Insipidus
The treatment for diabetes insipidus depends on the underlying cause. In cases of central diabetes insipidus, where there is a deficiency of ADH, treatment typically involves replacing the hormone through medications such as desmopressin. Desmopressin can be taken orally, as a nasal spray, or through injection.
For nephrogenic diabetes insipidus, treatment focuses on addressing the underlying cause and managing symptoms. This may involve adjusting medications, managing kidney disease, or making dietary changes to reduce fluid intake.
Living with Diabetes Insipidus
Living with diabetes insipidus can be challenging, but with proper management, individuals can lead normal lives. Here are some tips for managing the condition:
- Stay hydrated: It is important to drink enough fluids to prevent dehydration. Work with your healthcare provider to determine the appropriate amount of fluid intake for your specific needs.
- Monitor urine output: Keep track of your urine output to ensure it remains within a normal range. This can help identify any changes or potential complications.
- Wear a medical alert bracelet: In case of emergencies, wearing a medical alert bracelet that indicates your condition can help healthcare professionals provide appropriate care.
- Follow your treatment plan: Take medications as prescribed and attend regular check-ups with your healthcare provider to monitor your condition and make any necessary adjustments to your treatment plan.
Complications of Diabetes Insipidus
If diabetes insipidus is not properly managed, it can lead to various complications. These can include:
- Dehydration: Without adequate fluid intake, dehydration can occur, leading to dizziness, confusion, and even life-threatening situations.
- Electrolyte imbalances: Diabetes insipidus can disrupt the balance of electrolytes in the body, which can affect various bodily functions.
- Kidney damage: Chronic dehydration and electrolyte imbalances can put strain on the kidneys, potentially leading to kidney damage over time.
It is important to work closely with your healthcare provider to manage your condition and prevent these complications.
Conclusion
Diabetes insipidus is a rare condition that affects the body’s ability to regulate fluid balance. It is characterized by excessive thirst and the production of large amounts of diluted urine. While there is no cure for diabetes insipidus, it can be effectively managed through medications and lifestyle modifications. By understanding the causes, symptoms, and treatment options for diabetes insipidus, individuals can take control of their condition and lead fulfilling lives.