Exocrine pancreatic insufficiency (EPI) is a digestive disorder characterized by the inability of the pancreas to produce enough digestive enzymes. This condition, also known as pancreatic insufficiency or pancreatic enzyme deficiency, can lead to malabsorption and various symptoms related to poor digestion. In this article, we will explore the symptoms and treatment options for exocrine pancreatic insufficiency, shedding light on this often overlooked pancreatic disease.
Understanding Exocrine Pancreatic Insufficiency
The pancreas plays a crucial role in the digestive process by producing enzymes that help break down fats, proteins, and carbohydrates. In individuals with EPI, the pancreas fails to produce enough of these enzymes, leading to malabsorption and nutrient deficiencies.
EPI can be caused by various factors, including chronic pancreatitis, cystic fibrosis, pancreatic cancer, and certain genetic conditions. It can also occur as a result of surgical removal of the pancreas or its dysfunction due to autoimmune diseases.
Recognizing the Symptoms of EPI
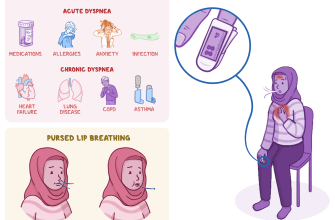
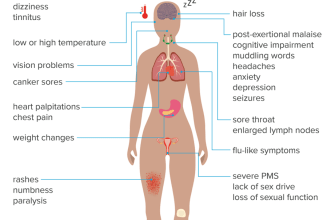
Exocrine pancreatic insufficiency can manifest through a range of symptoms, which may vary in severity from person to person. Some common symptoms include:
- Steatorrhea: This refers to the passage of pale, bulky, and foul-smelling stools due to the malabsorption of fats.
- Weight loss: Inadequate digestion and absorption of nutrients can lead to unintentional weight loss.
- Abdominal pain: Some individuals with EPI may experience abdominal pain or discomfort, often after eating.
- Bloating and gas: The inability to properly digest food can result in excessive gas production and bloating.
- Malnutrition: EPI can lead to nutrient deficiencies, causing symptoms such as fatigue, weakness, and vitamin deficiencies.
If you experience any of these symptoms, it is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
Diagnosing Exocrine Pancreatic Insufficiency
Diagnosing EPI involves a combination of medical history evaluation, physical examination, and diagnostic tests. Your healthcare provider may ask about your symptoms, perform a physical examination, and order specific tests to confirm the diagnosis.
Some common diagnostic tests for EPI include:
- Fecal elastase test: This test measures the levels of elastase, an enzyme produced by the pancreas, in the stool. Low levels indicate pancreatic insufficiency.
- Secretin stimulation test: This test involves the administration of secretin, a hormone that stimulates the pancreas to release digestive enzymes. The levels of enzymes in the duodenal fluid are then measured.
- Endoscopic ultrasound: This procedure uses an ultrasound probe inserted through the mouth to obtain detailed images of the pancreas and surrounding structures.
These tests, along with other clinical evaluations, help determine the presence and severity of exocrine pancreatic insufficiency.
Treatment Options for EPI
While exocrine pancreatic insufficiency cannot be cured, it can be effectively managed with appropriate treatment. The primary goal of treatment is to replace the deficient pancreatic enzymes and alleviate symptoms.
Pancreatic Enzyme Replacement Therapy (PERT)
The cornerstone of EPI treatment is pancreatic enzyme replacement therapy (PERT). PERT involves taking pancreatic enzyme supplements with meals to aid digestion. These supplements contain lipase, amylase, and protease enzymes, which help break down fats, carbohydrates, and proteins, respectively.
Pancreatic enzyme supplements are available in various forms, including capsules and tablets. Your healthcare provider will determine the appropriate dosage based on your specific needs. It is important to take these supplements as prescribed and with every meal or snack to ensure optimal digestion.
Dietary Modifications
In addition to PERT, dietary modifications can play a significant role in managing EPI symptoms. Some dietary recommendations for individuals with EPI include:
- Consuming smaller, more frequent meals to aid digestion
- Avoiding high-fat foods that may exacerbate symptoms
- Including lean proteins, fruits, vegetables, and whole grains in the diet
- Working with a registered dietitian to develop a personalized meal plan
It is important to note that dietary modifications should be tailored to individual needs and preferences. Consulting a healthcare professional or registered dietitian can provide valuable guidance in this regard.
Managing Underlying Conditions
If EPI is caused by an underlying condition, such as chronic pancreatitis or cystic fibrosis, managing and treating the underlying condition is crucial. This may involve medications, lifestyle changes, and other interventions specific to the underlying condition.
Conclusion
Exocrine pancreatic insufficiency is a digestive disorder characterized by the inadequate production of pancreatic enzymes. It can lead to malabsorption, weight loss, abdominal pain, and other symptoms. While EPI cannot be cured, it can be effectively managed through pancreatic enzyme replacement therapy, dietary modifications, and addressing any underlying conditions. If you suspect you may have EPI, it is important to seek medical attention for an accurate diagnosis and appropriate treatment.