Hemolysis refers to the destruction of red blood cells in the body. This condition can be caused by various factors and can lead to a range of symptoms. Understanding the causes, symptoms, and treatment options for hemolysis is crucial for effective management and prevention of complications. In this article, we will explore the different aspects of hemolysis and provide valuable insights into its diagnosis, treatment, and prevention.
Causes of Hemolysis
Hemolysis can occur due to several underlying causes, including:
- Autoimmune disorders: Conditions such as autoimmune hemolytic anemia can cause the immune system to mistakenly attack and destroy red blood cells.
- Infections: Certain infections, such as malaria or bacterial infections, can trigger hemolysis.
- Medications: Some medications, including certain antibiotics and antimalarial drugs, can induce hemolysis as a side effect.
- Genetic disorders: Inherited conditions like sickle cell disease or hereditary spherocytosis can lead to abnormal red blood cells that are more prone to destruction.
- Toxins: Exposure to certain toxins, such as snake venom or chemicals, can cause hemolysis.
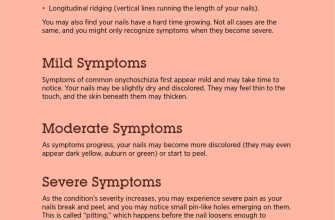
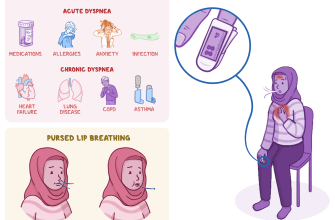
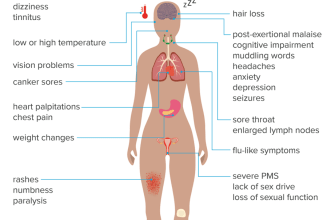
Symptoms of Hemolysis
The symptoms of hemolysis can vary depending on the severity of the condition. Some common signs and symptoms include:
- Fatigue and weakness
- Shortness of breath
- Pale skin or jaundice
- Dark urine
- Enlarged spleen
- Increased heart rate
- Abdominal pain
If you experience any of these symptoms, it is important to consult a healthcare professional for a proper diagnosis and appropriate treatment.
Hemolysis Diagnosis
Diagnosing hemolysis involves a combination of medical history evaluation, physical examination, and laboratory tests. Your healthcare provider may perform the following:
- Complete blood count (CBC): This test measures the number of red blood cells, white blood cells, and platelets in your blood.
- Peripheral blood smear: A sample of your blood is examined under a microscope to check for any abnormalities in the red blood cells.
- Direct Coombs test: This test helps determine if your hemolysis is caused by an autoimmune reaction.
- Hemoglobin electrophoresis: This test is used to identify abnormal types of hemoglobin that may be causing hemolysis.
Based on the results of these tests, your healthcare provider can make an accurate diagnosis and recommend appropriate treatment options.
Hemolysis Treatment
The treatment of hemolysis depends on the underlying cause and the severity of the condition. Some common treatment options include:
- Medications: In cases of autoimmune hemolytic anemia, immunosuppressive drugs may be prescribed to suppress the immune system and reduce red blood cell destruction.
- Blood transfusions: In severe cases of hemolysis, blood transfusions may be necessary to replace the destroyed red blood cells and improve oxygen delivery to the body.
- Splenectomy: If an enlarged spleen is causing excessive red blood cell destruction, surgical removal of the spleen may be recommended.
- Treating underlying infections or diseases: If hemolysis is secondary to an infection or an underlying medical condition, treating the root cause can help alleviate the symptoms.
It is important to note that the treatment of hemolysis should be tailored to each individual’s specific needs and should be carried out under the guidance of a healthcare professional.
Hemolysis Prevention and Management
While it may not always be possible to prevent hemolysis, there are certain measures that can help reduce the risk and manage the condition effectively:
- Avoid triggers: If you have a known trigger for hemolysis, such as certain medications or toxins, it is important to avoid them to prevent further red blood cell destruction.
- Stay hydrated: Drinking an adequate amount of water can help maintain the health and integrity of red blood cells.
- Follow a balanced diet: Consuming a diet rich in iron, vitamin B12, and folate can support red blood cell production and reduce the risk of hemolysis.
- Regular check-ups: Routine medical check-ups can help detect any underlying conditions or infections that may contribute to hemolysis.
By following these preventive measures and effectively managing any underlying conditions, individuals can minimize the risk of hemolysis and its associated complications.
Hemolysis Complications and Research
If left untreated or poorly managed, hemolysis can lead to various complications, including:
- Anemia: The destruction of red blood cells can result in a decrease in the number of healthy red blood cells, leading to anemia.
- Organ damage: In severe cases, hemolysis can cause damage to organs such as the kidneys or liver.
- Increased risk of infections: Hemolysis can weaken the immune system, making individuals more susceptible to infections.
Researchers are continuously studying hemolysis to better understand its causes, develop more effective treatment options, and improve patient outcomes. Ongoing research aims to identify new therapeutic targets and interventions that can help manage hemolysis more efficiently.
In conclusion, hemolysis is a condition characterized by the destruction of red blood cells. It can be caused by various factors and can lead to a range of symptoms. Timely diagnosis, appropriate treatment, and preventive measures are essential for managing hemolysis effectively and preventing complications. By following the guidance of healthcare professionals and adopting a healthy lifestyle, individuals can minimize the impact of hemolysis on their overall well-being.