Steatorrhea, also known as fatty stool, is a condition characterized by the presence of excessive fat in the stool. This can be caused by various factors and can lead to a range of symptoms and complications. In this article, we will explore the causes of steatorrhea, its symptoms, diagnosis, treatment options, management strategies, prevention methods, and the importance of a steatorrhea diet.
Causes of Steatorrhea
Steatorrhea can be caused by several underlying conditions and factors. Some of the common causes include:
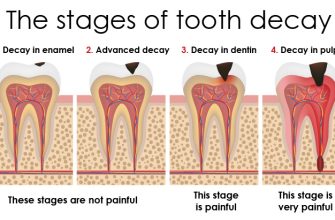
- Pancreatic disorders: Conditions such as chronic pancreatitis, pancreatic cancer, and cystic fibrosis can affect the production and secretion of pancreatic enzymes, which are essential for fat digestion. Without sufficient enzymes, fat cannot be properly broken down and absorbed, leading to steatorrhea.
- Gallbladder dysfunction: The gallbladder stores bile, which is necessary for the digestion and absorption of fat. If the gallbladder is not functioning properly, bile production may be impaired, resulting in steatorrhea.
- Small intestine disorders: Diseases like celiac disease, Crohn’s disease, and bacterial overgrowth in the small intestine can interfere with fat absorption, leading to steatorrhea.
- Medications: Certain medications, such as orlistat (a weight loss drug) and some antibiotics, can interfere with fat absorption and cause steatorrhea as a side effect.
Symptoms of Steatorrhea
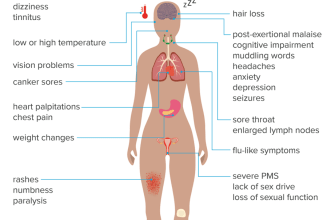
The main symptom of steatorrhea is the presence of bulky, greasy, and foul-smelling stools. Other common symptoms include:
- Diarrhea
- Abdominal pain or cramps
- Weight loss
- Malnutrition
- Vitamin deficiencies (especially fat-soluble vitamins like A, D, E, and K)
Diagnosis of Steatorrhea
To diagnose steatorrhea, a healthcare professional may perform the following tests:
- Stool analysis: A sample of the stool is examined for the presence of fat using a special stain. If the fat content exceeds a certain threshold, steatorrhea is diagnosed.
- Blood tests: Blood tests may be conducted to check for nutritional deficiencies and assess pancreatic and liver function.
- Imaging tests: Imaging techniques like ultrasound, CT scan, or MRI may be used to evaluate the pancreas, gallbladder, and small intestine for any abnormalities.
- Endoscopy: In some cases, an endoscopy may be performed to directly visualize the small intestine and obtain tissue samples for further analysis.
Treatment of Steatorrhea
The treatment of steatorrhea depends on the underlying cause. Some common treatment options include:
- Enzyme replacement therapy: If the steatorrhea is caused by pancreatic enzyme deficiency, enzyme supplements can be prescribed to aid in fat digestion. These supplements are taken with meals to ensure proper absorption of fats.
- Gallbladder surgery: If gallbladder dysfunction is the cause of steatorrhea, surgical removal of the gallbladder (cholecystectomy) may be recommended.
- Management of underlying conditions: Treating the underlying conditions, such as celiac disease or Crohn’s disease, can help improve fat absorption and reduce steatorrhea.
- Dietary modifications: Following a steatorrhea diet can help manage symptoms and improve fat absorption. This may involve reducing fat intake, increasing fiber consumption, and avoiding foods that worsen symptoms.
Management and Prevention of Steatorrhea
Managing and preventing steatorrhea involves a combination of lifestyle changes and medical interventions. Here are some strategies:
- Follow a steatorrhea diet: A low-fat, high-fiber diet can help manage symptoms and improve fat absorption. This includes consuming lean proteins, whole grains, fruits, and vegetables, while limiting fatty and fried foods.
- Take enzyme supplements: If pancreatic enzyme deficiency is the cause of steatorrhea, taking enzyme supplements as prescribed by a healthcare professional can aid in fat digestion.
- Manage underlying conditions: Properly managing conditions like celiac disease or Crohn’s disease can help prevent steatorrhea or reduce its severity.
- Stay hydrated: Drinking an adequate amount of water can help prevent dehydration, which is common in individuals with steatorrhea due to increased fluid loss through diarrhea.
- Regular follow-ups: Regular check-ups with a healthcare professional are important to monitor the progress of treatment and make any necessary adjustments.
Complications of Steatorrhea
If left untreated, steatorrhea can lead to various complications, including:
- Malnutrition: Inadequate absorption of fats can result in malnutrition, as essential nutrients are not properly absorbed by the body.
- Vitamin deficiencies: Steatorrhea can lead to deficiencies in fat-soluble vitamins, which are necessary for various bodily functions.
- Osteoporosis: Vitamin D deficiency, often associated with steatorrhea, can lead to weakened bones and an increased risk of fractures.
- Weight loss: Steatorrhea can cause unintentional weight loss due to malabsorption of nutrients.
In conclusion, steatorrhea is a condition characterized by the presence of excessive fat in the stool. It can be caused by various factors, including pancreatic disorders, gallbladder dysfunction, small intestine disorders, and certain medications. The main symptom is the presence of bulky, greasy stools, along with other digestive symptoms. Diagnosis involves stool analysis, blood tests, imaging tests, and endoscopy. Treatment options include enzyme replacement therapy, gallbladder surgery, management of underlying conditions, and dietary modifications. Managing and preventing steatorrhea involves following a steatorrhea diet, taking enzyme supplements, managing underlying conditions, staying hydrated, and regular follow-ups. If left untreated, steatorrhea can lead to complications such as malnutrition, vitamin deficiencies, osteoporosis, and weight loss. Therefore, it is important to seek medical attention and follow the recommended treatment plan to effectively manage this condition.