Hemolytic anemia is a condition characterized by the destruction of red blood cells at a rate faster than their production. This can lead to a decrease in the number of red blood cells in the body, resulting in various symptoms and complications. Understanding the causes, symptoms, and treatment options for hemolytic anemia is crucial for effective management and prevention of this condition.
Causes of Hemolytic Anemia
Hemolytic anemia can be caused by various factors, including:
- Autoimmune disorders: In autoimmune hemolytic anemia, the body’s immune system mistakenly attacks and destroys its own red blood cells.
- Infections: Certain infections, such as malaria or bacterial infections, can trigger the destruction of red blood cells.
- Medications: Some medications, such as certain antibiotics or antimalarial drugs, can cause hemolytic anemia as a side effect.
- Genetic disorders: Inherited conditions like sickle cell anemia or thalassemia can lead to the destruction of red blood cells.
- Toxins: Exposure to certain toxins, such as lead or snake venom, can cause hemolytic anemia.
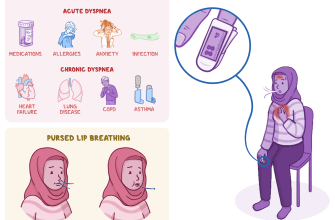
Symptoms of Hemolytic Anemia
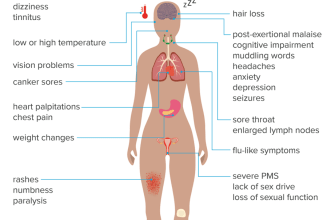
The symptoms of hemolytic anemia can vary depending on the severity of the condition. Common symptoms include:
- Fatigue and weakness
- Shortness of breath
- Pale skin
- Rapid heart rate
- Jaundice (yellowing of the skin and eyes)
- Dark urine
- Enlarged spleen
If you experience any of these symptoms, it is important to consult a healthcare professional for a proper diagnosis and treatment.
Diagnosis of Hemolytic Anemia
To diagnose hemolytic anemia, your doctor may perform various tests, including:
- Complete blood count (CBC): This test measures the number of red blood cells, white blood cells, and platelets in your blood.
- Peripheral blood smear: A sample of your blood is examined under a microscope to check for abnormalities in the shape and size of red blood cells.
- Coomb’s test: This test detects the presence of antibodies or complement proteins on the surface of red blood cells.
- Bone marrow biopsy: In some cases, a small sample of bone marrow may be taken to determine the underlying cause of hemolytic anemia.
Types of Hemolytic Anemia
There are several types of hemolytic anemia, including:
- Autoimmune hemolytic anemia
- Hereditary spherocytosis
- Sickle cell anemia
- Thalassemia
- G6PD deficiency
Each type has its own specific causes and treatment options, so an accurate diagnosis is essential for effective management.
Treatment for Hemolytic Anemia
The treatment for hemolytic anemia depends on the underlying cause and severity of the condition. Some common treatment options include:
- Medications: Corticosteroids or immunosuppressive drugs may be prescribed to suppress the immune system and reduce the destruction of red blood cells in autoimmune hemolytic anemia.
- Blood transfusions: In severe cases, blood transfusions may be necessary to increase the number of red blood cells in the body.
- Splenectomy: Surgical removal of the spleen may be recommended in certain cases to prevent the destruction of red blood cells.
- Folic acid supplements: Folic acid is essential for red blood cell production, and supplements may be prescribed to support their growth.
It is important to work closely with your healthcare provider to determine the most appropriate treatment plan for your specific condition.
Management of Hemolytic Anemia
In addition to medical treatment, there are several ways to manage hemolytic anemia and reduce the risk of complications:
- Avoid triggers: If your hemolytic anemia is triggered by certain medications or toxins, it is important to avoid exposure to these substances.
- Stay hydrated: Drinking plenty of fluids can help prevent dehydration, which can worsen the symptoms of anemia.
- Eat a balanced diet: Consuming foods rich in iron, vitamin B12, and folic acid can support red blood cell production.
- Manage underlying conditions: If your hemolytic anemia is caused by an underlying condition, such as an autoimmune disorder, managing that condition effectively can help control the destruction of red blood cells.
Complications of Hemolytic Anemia
If left untreated or poorly managed, hemolytic anemia can lead to various complications, including:
- Heart problems: Anemia can strain the heart, leading to an increased risk of heart failure or irregular heart rhythms.
- Gallstones: The breakdown of red blood cells can release excess bilirubin, which can contribute to the formation of gallstones.
- Organ damage: Severe anemia can deprive organs of oxygen, potentially causing damage to the brain, heart, and other vital organs.
Early diagnosis and appropriate treatment can help prevent these complications and improve overall health outcomes.
Prevention of Hemolytic Anemia
While some types of hemolytic anemia are genetic and cannot be prevented, there are steps you can take to reduce the risk of acquired forms of the condition:
- Avoid exposure to toxins: Be cautious of exposure to chemicals, medications, or substances known to cause hemolytic anemia.
- Practice good hygiene: Taking steps to prevent infections, such as washing hands regularly and getting vaccinated, can reduce the risk of infection-related hemolytic anemia.
- Follow medication instructions: If you are taking medications known to cause hemolytic anemia, follow the prescribed dosage and consult your healthcare provider if you experience any unusual symptoms.
By being proactive and taking preventive measures, you can minimize the risk of developing hemolytic anemia.
In conclusion, hemolytic anemia is a condition characterized by the destruction of red blood cells at a faster rate than their production. It can be caused by various factors, including autoimmune disorders, infections, medications, genetic disorders, and toxins. The symptoms of hemolytic anemia can vary but commonly include fatigue, shortness of breath, pale skin, and jaundice. Diagnosis involves various tests, and treatment options depend on the underlying cause and severity of the condition. Managing hemolytic anemia involves avoiding triggers, staying hydrated, eating a balanced diet, and managing underlying conditions. Early diagnosis and appropriate treatment are essential to prevent complications and improve overall health. By following preventive measures, you can reduce the risk of acquiring hemolytic anemia. If you experience any symptoms or have concerns, it is important to consult a healthcare professional for proper evaluation and guidance.