Osteomyelitis is a serious bone infection that can cause severe pain and discomfort. It occurs when bacteria or fungi enter the bone, leading to inflammation and infection. If left untreated, osteomyelitis can result in long-term complications and even life-threatening conditions. In this article, we will explore the symptoms, treatment options, and prevention strategies for osteomyelitis.
Osteomyelitis Causes
Osteomyelitis can be caused by various factors, including:
- Bacterial or fungal infections: The most common cause of osteomyelitis is a bacterial infection, often resulting from an open wound or surgery. Fungal infections can also lead to osteomyelitis, although they are less common.
- Bloodstream infections: Bacteria or fungi can enter the bloodstream and spread to the bones, causing osteomyelitis. This is more common in individuals with weakened immune systems or those who use intravenous drugs.
- Contiguous spread: In some cases, infections from nearby tissues, such as skin or muscles, can spread to the bones and cause osteomyelitis.
Osteomyelitis Symptoms
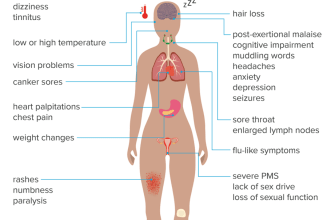
The symptoms of osteomyelitis can vary depending on the severity and location of the infection. Common symptoms include:
- Severe pain and tenderness in the affected area
- Swelling, redness, and warmth around the infected bone
- Fever and chills
- Fatigue and general malaise
- Difficulty moving the affected limb
- Pus or drainage from the infected area
If you experience any of these symptoms, it is important to seek medical attention promptly. Early diagnosis and treatment can help prevent complications and improve outcomes.
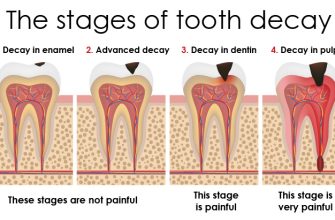
Osteomyelitis Diagnosis
Diagnosing osteomyelitis typically involves a combination of medical history review, physical examination, and diagnostic tests. Your doctor may:
- Ask about your symptoms, medical history, and any recent injuries or surgeries
- Perform a physical examination to assess the affected area for signs of infection
- Order blood tests to check for elevated white blood cell count and markers of inflammation
- Conduct imaging tests, such as X-rays, MRI, or CT scans, to visualize the affected bone and surrounding tissues
- Collect a sample of bone or tissue for laboratory analysis to identify the specific bacteria or fungi causing the infection
Once a diagnosis is confirmed, your doctor will determine the appropriate treatment plan based on the severity and location of the infection.
Osteomyelitis Treatment
The treatment of osteomyelitis typically involves a combination of antibiotics, surgical intervention, and supportive care. The specific approach may vary depending on the individual case.
Antibiotics
Antibiotics are the primary treatment for osteomyelitis caused by bacterial infections. The choice of antibiotics will depend on the type of bacteria identified through laboratory analysis. Intravenous antibiotics are often administered initially to ensure high levels of medication reach the infected bone. Oral antibiotics may be prescribed for a prolonged period to complete the course of treatment.
Surgical Intervention
In some cases, surgical intervention may be necessary to remove infected tissue, drain abscesses, or repair damaged bones. Surgery can help improve the effectiveness of antibiotics and promote healing. It may involve procedures such as debridement, bone grafting, or the placement of antibiotic beads.
Supportive Care
Supportive care measures can help manage symptoms and promote recovery. These may include pain management, physical therapy, and wound care. It is essential to follow your healthcare provider’s instructions and complete the full course of treatment to ensure successful recovery.
Osteomyelitis Prevention
Preventing osteomyelitis involves taking steps to reduce the risk of infection. Some preventive measures include:
- Maintaining good hygiene: Properly clean and care for wounds to prevent bacterial or fungal infections.
- Managing chronic conditions: If you have a chronic condition that increases the risk of osteomyelitis, such as diabetes or peripheral artery disease, work closely with your healthcare provider to manage it effectively.
- Practicing safe injection practices: If you use intravenous drugs, seek help to quit and practice safe injection techniques to reduce the risk of bloodstream infections.
- Following surgical protocols: If you undergo surgery, follow all post-operative instructions to minimize the risk of infection.
Osteomyelitis Complications
Without prompt and appropriate treatment, osteomyelitis can lead to several complications, including:
- Chronic infection: Osteomyelitis can become a long-term or recurring condition, requiring ongoing treatment and management.
- Bone death (sequestrum): In severe cases, the infected bone may die, leading to the formation of dead tissue within the bone.
- Joint damage: Osteomyelitis can affect nearby joints, leading to arthritis and limited mobility.
- Spread of infection: If left untreated, the infection can spread to other parts of the body, potentially causing life-threatening conditions.
Osteomyelitis Risk Factors
Several factors can increase the risk of developing osteomyelitis, including:
- Diabetes
- Peripheral artery disease
- Recent trauma or surgery
- Compromised immune system
- Intravenous drug use
- Chronic steroid use
If you have any of these risk factors, it is important to be vigilant and seek medical attention promptly if you suspect an infection.
In conclusion, osteomyelitis is a serious bone infection that requires early diagnosis and appropriate treatment. By understanding the causes, symptoms, treatment options, and prevention strategies, individuals can take proactive steps to protect their bone health and overall well-being.