Myoclonus is a neurological disorder characterized by sudden, brief muscle spasms or involuntary muscle contractions. These muscle jerks can occur in various parts of the body and can range from mild to severe. In this article, we will explore the causes of myoclonus, its symptoms, types, diagnosis, and available treatment options.
Causes of Myoclonus
Myoclonus can have several underlying causes, including:
- Genetic factors: Some forms of myoclonus are inherited and can be passed down through generations.
- Brain damage: Traumatic brain injury, stroke, or other conditions that affect the brain can lead to myoclonus.
- Metabolic disorders: Certain metabolic disorders, such as liver or kidney failure, can trigger myoclonus.
- Medications: Some medications, particularly those used to treat epilepsy or psychiatric disorders, can cause myoclonus as a side effect.
- Toxic exposure: Exposure to certain toxins, such as carbon monoxide or heavy metals, can result in myoclonus.
Types of Myoclonus
There are various types of myoclonus, each with its own characteristics:
Physiological Myoclonus
Physiological myoclonus is considered normal and can occur in healthy individuals. Examples include hiccups or the sudden jerk experienced when falling asleep.
Epileptic Myoclonus
Epileptic myoclonus is associated with epilepsy and is characterized by muscle jerks that are triggered by abnormal electrical activity in the brain.
Essential Myoclonus
Essential myoclonus is a primary form of myoclonus, meaning it is not caused by an underlying condition. The exact cause of essential myoclonus is unknown.
Secondary Myoclonus
Secondary myoclonus is caused by an underlying condition or factor, such as brain damage, medication side effects, or metabolic disorders.
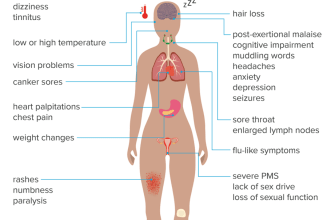
Myoclonus Symptoms
The main symptom of myoclonus is the sudden, involuntary muscle contractions or spasms. These jerks can occur in any muscle group and may be isolated or repetitive. Other symptoms may include:
- Difficulty with coordination and balance
- Impaired speech
- Tremors
- Difficulty swallowing
- Uncontrollable movements of the limbs
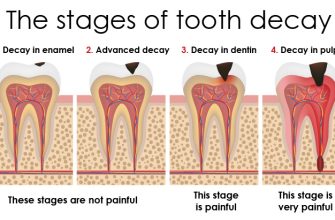
Myoclonus Diagnosis
Diagnosing myoclonus involves a thorough evaluation of the patient’s medical history, physical examination, and possibly additional tests. The doctor may perform:
- Electromyography (EMG): This test measures the electrical activity of the muscles and can help determine the type and severity of myoclonus.
- Brain imaging: MRI or CT scans may be used to identify any structural abnormalities in the brain.
- Blood tests: These can help identify any underlying metabolic disorders or toxic exposures.
Treatment for Myoclonus
While there is no cure for myoclonus, treatment aims to manage symptoms and improve quality of life. The approach to treatment may vary depending on the underlying cause and severity of myoclonus. Some treatment options include:
- Medications: Certain medications, such as anti-seizure drugs or muscle relaxants, may help reduce the frequency and intensity of myoclonic jerks.
- Physical therapy: Exercises and stretching can help improve muscle control and reduce the impact of myoclonus on daily activities.
- Deep brain stimulation: In severe cases, deep brain stimulation may be considered. This involves implanting electrodes in the brain to regulate abnormal electrical activity.
- Lifestyle modifications: Avoiding triggers, such as certain medications or substances, can help minimize myoclonus episodes.
It is important for individuals with myoclonus to work closely with their healthcare team to develop a personalized treatment plan that addresses their specific needs and goals.
Managing Myoclonus
Living with myoclonus can be challenging, but there are strategies that can help manage the condition:
- Establish a routine: Maintaining a consistent daily routine can help minimize stress and potential triggers.
- Practice relaxation techniques: Techniques such as deep breathing, meditation, or yoga can help reduce muscle tension and promote relaxation.
- Seek support: Joining support groups or connecting with others who have myoclonus can provide valuable emotional support and practical tips for coping.
- Adapt the environment: Making modifications to the living space, such as removing trip hazards or using assistive devices, can help prevent falls or injuries during myoclonus episodes.
In conclusion, myoclonus is a neurological disorder characterized by involuntary muscle contractions or spasms. It can have various causes, including genetic factors, brain damage, medications, or toxic exposure. While there is no cure, treatment options such as medications, physical therapy, and lifestyle modifications can help manage symptoms and improve quality of life. By working closely with healthcare professionals and implementing strategies to cope with myoclonus, individuals can lead fulfilling lives despite the challenges posed by this condition.