Fractures, or broken bones, are a common occurrence that can happen to anyone at any age. While some fractures are the result of accidents or trauma, others may occur due to underlying medical conditions or lifestyle factors. Understanding the causes of frequent fractures and how to treat them is essential for preventing further injury and promoting proper healing.
Types of Fractures
Fractures can be classified into several types, each with its own characteristics and treatment approach:
1. Closed Fracture
A closed fracture refers to a broken bone that does not penetrate the skin. It is often caused by a direct blow or trauma to the bone.
2. Open Fracture
An open fracture, also known as a compound fracture, occurs when the broken bone pierces through the skin. This type of fracture carries a higher risk of infection and requires immediate medical attention.
3. Stress Fracture
A stress fracture is a hairline crack in the bone that develops over time due to repetitive stress or overuse. Athletes and individuals who engage in high-impact activities are more prone to stress fractures.
4. Greenstick Fracture
A greenstick fracture is a partial break in the bone, commonly seen in children whose bones are more flexible than adults. The bone bends and cracks but does not completely break.
5. Comminuted Fracture
A comminuted fracture occurs when the bone breaks into multiple fragments. This type of fracture is often caused by high-energy trauma, such as a car accident or a fall from a significant height.
Causes of Frequent Fractures
Several factors can contribute to frequent fractures:
1. Osteoporosis
Osteoporosis is a condition characterized by low bone density and increased bone fragility. It is more common in older adults, particularly women after menopause. Weakening of the bones due to osteoporosis can lead to frequent fractures, even with minimal trauma.
2. Vitamin D and Calcium Deficiency
Vitamin D and calcium are essential for maintaining strong and healthy bones. Deficiencies in these nutrients can weaken the bones, making them more susceptible to fractures.
3. Genetic Factors
Some individuals may have a genetic predisposition to weaker bones, making them more prone to fractures. Conditions like osteogenesis imperfecta, also known as brittle bone disease, can cause frequent fractures from a young age.
4. Certain Medications
Long-term use of certain medications, such as corticosteroids, can weaken the bones and increase the risk of fractures.
5. Falls and Accidents
Falls and accidents are common causes of fractures, especially in older adults. Weak muscles, poor balance, and environmental hazards can contribute to falls and subsequent fractures.
Fracture Symptoms and Diagnosis
The symptoms of a fracture may vary depending on the location and severity of the injury. Common signs of a fracture include:
- Pain and tenderness at the site of the fracture
- Swelling and bruising
- Deformity or abnormal positioning of the affected limb
- Inability to bear weight or use the injured limb
If a fracture is suspected, a healthcare professional will perform a thorough physical examination and may order diagnostic tests, such as X-rays or MRI scans, to confirm the diagnosis and determine the extent of the injury.
Fracture Treatment and Management
The treatment and management of fractures depend on various factors, including the type and location of the fracture, as well as the individual’s overall health. Common approaches to fracture treatment include:
1. Immobilization
Immobilization involves keeping the fractured bone in place to promote healing. This may be achieved through the use of casts, splints, or braces. Immobilization helps to stabilize the bone and prevent further damage.
2. Medications
Pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may be prescribed to manage pain and reduce inflammation associated with fractures. In some cases, medications to promote bone healing, such as bisphosphonates, may also be recommended.
3. Surgery
In certain fractures, surgery may be necessary to realign the bones and stabilize them with the use of screws, plates, or rods. This is often the case for complex fractures or fractures that do not heal properly with conservative treatment.
4. Rehabilitation
After the initial healing phase, rehabilitation plays a crucial role in restoring strength, mobility, and function to the affected limb. Physical therapy exercises and techniques help to improve muscle strength, joint flexibility, and overall recovery.
Fracture Prevention
While not all fractures can be prevented, there are steps individuals can take to reduce their risk:
1. Maintain a Healthy Diet
A well-balanced diet rich in calcium and vitamin D is essential for maintaining strong bones. Include dairy products, leafy greens, and fortified foods in your diet to ensure an adequate intake of these nutrients.
2. Exercise Regularly
Weight-bearing exercises, such as walking or jogging, and strength training can help improve bone density and strength. Engaging in regular physical activity also improves balance and coordination, reducing the risk of falls.
3. Fall Prevention
Take precautions to prevent falls, especially in older adults. Remove tripping hazards from your home, install handrails on stairs, and use appropriate lighting to improve visibility.
4. Avoid Smoking and Excessive Alcohol Consumption
Smoking and excessive alcohol consumption can weaken the bones and increase the risk of fractures. Quit smoking and limit alcohol intake to promote bone health.
Fracture Healing Process
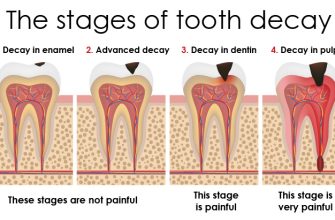
The healing process of a fracture typically involves several stages:
1. Inflammatory Phase
Immediately after a fracture, the body initiates an inflammatory response to remove damaged tissue and prepare the site for healing. This phase lasts for a few days.
2. Soft Callus Formation
Within a week or two, a soft callus made of collagen and cartilage forms around the fracture site. This provides initial stability and support.
3. Hard Callus Formation
Over the next several weeks, the soft callus is gradually replaced by a hard callus made of new bone tissue. This process is known as callus formation.
4. Remodeling Phase
Over several months, the newly formed bone undergoes remodeling, where it is reshaped and strengthened to restore its original structure and strength.
It is important to note that the healing time for fractures can vary depending on various factors, including the individual’s age, overall health, and the type of fracture.
In conclusion, frequent fractures can be caused by various factors, including underlying medical conditions, lifestyle choices, and accidents. Prompt diagnosis and appropriate treatment are crucial for proper healing and preventing further injury. By understanding the causes, symptoms, and treatment options for fractures, individuals can take steps to prevent fractures and promote bone health.